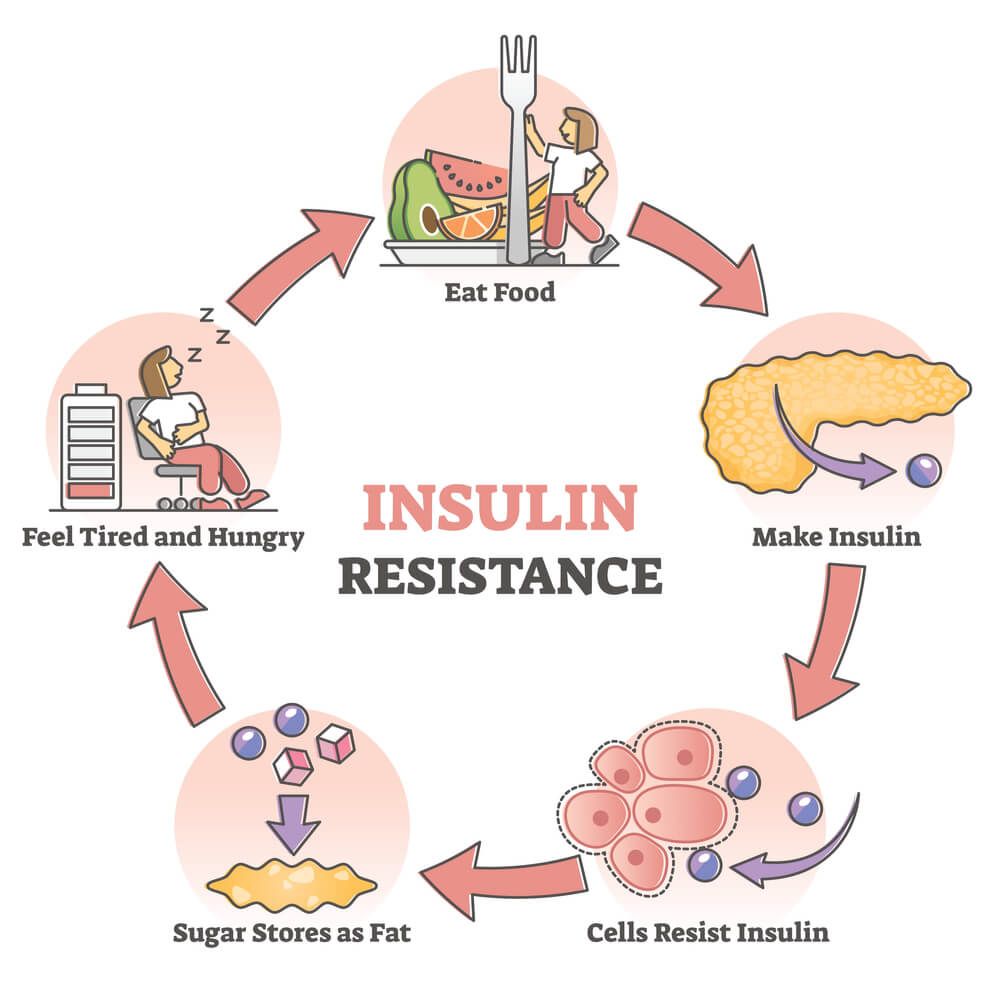
Insulin is a hormone, released by the pancreas in response to increased blood sugar levels. The job of insulin is to enable glucose to enter your muscle, fat and liver tissue, where it can be used for energy or storage. After a meal, as blood sugar rises, insulin is released, allowing glucose to move out of the blood, and stabilizing blood sugar levels. Insulin sensitivity refers to how sensitive the body tissue is to insulin. A person with low insulin sensitivity has insulin resistance and is at higher risk of developing type 2 diabetes.
Fatigue, weight gain, brain fog, increased hunger, frequent infections and increased thirst are all symptoms of insulin resistance. Untreated insulin resistance can even lead to type 2 diabetes. Diet and lifestyle changes can have a major impact on insulin resistance.
What Exactly is Insulin Resistance?
Insulin resistance occurs when your cells do not respond well to insulin, meaning that your tissues can not take up glucose as well as they should. To compensate, your pancreas continues to pump out more insulin to keep the blood glucose in the normal range. This can help in the short term, but in the long term the pancreas cannot keep up with the demand, leading to prediabetes and type 2 diabetes.
What Causes Insulin Resistance?
There is not one cause of insulin resistance, instead, it seems to be due to a number of lifestyles, environmental and genetic factors. Many of these also contribute to what is known as metabolic syndrome, or overall metabolic dysfunction in the body. Metabolic syndrome is defined by high blood sugar, low levels of HDL (good cholesterol), high levels of triglycerides, an increased waist circumference, and high blood pressure.
All of these factors together increase a person’s risk of developing a number of conditions including cardiovascular disease, diabetes, stroke and other cardiovascular conditions.
Excess Weight
Increased weight is strongly associated with insulin resistance. Not only is a higher weight a risk factor for insulin resistance, but insulin resistance can also lead to weight gain. This is because the cells can not respond to the rise in blood sugar levels, causing more glucose to be stored as fat. Fat concentrated in the midsection, known as visceral fat, is most associated with insulin resistance. A waist circumference of greater than 40 inches for men or 36 inches for women is strongly associated with insulin resistance. If the cells can not respond to the rise in blood sugar levels it will cause more glucose to be stored as fat.
Physical Inactivity
A sedentary lifestyle or decreased physical activity is also associated with insulin resistance. Regular physical activity has been shown to increase insulin sensitivity and reduce inflammation, both playing a role in the prevention of insulin resistance and diabetes.
Genetic Factors
Genetic factors such as a family history of type 2 diabetes and insulin resistance can also increase your risk. However, it is important to remember that lifestyle factors such as diet, exercise, sleep and stress management are the main determinants of metabolic health.
Acute and Chronic Stress
Both acute and chronic stress have also been associated with metabolic syndrome and the development of insulin resistance. This is due to the rise in cortisol that is triggered by stress. Cortisol causes an increase in both blood glucose levels and insulin levels, leading to an increased risk of developing insulin resistance.
Other Causes
Insulin resistance is associated with a number of other conditions, including, but not limited to:
- Polycystic Ovarian Syndrome (PCOS)
- High blood pressure
- Gestational diabetes
- Fatty liver disease
- Cushing’s syndrome
- Acromegaly
- Sleep Apnea
- Long-term glucocorticoid use
What Are the Risk Factors for Insulin Resistance?
Risk factors for insulin resistance include:
- Overweight or obese (BMI over 25)
- 45 years or older
- Family history of diabetes
- Ethnicity (African America, Hispanic, American Indian, Asian America, Hispanic or Latino)
- High blood pressure
- High cholesterol
- History of gestational diabetes
- Personal history of heart attack or stroke
- Polycystic Ovarian Syndrom (PCOS)
What Are the Symptoms of Insulin Resistance?
Symptoms of insulin resistance can be similar to those of prediabetes and diabetes. These include:
- Increased thirst or hunger
- Hunger, even after a meal
- Increased urination
- Tingling in the hands or feet
- Feeling tired or fatigued
- Frequent infections
Blood Work for Diagnosis of Insulin Resistance
Bloodwork can be a useful tool in the assessment and diagnosis of insulin resistance. Some blood work markers that are associated with insulin resistance include:
Hemoglobin A1c (HbA1c): Your HbA1c shows your average blood sugar levels over the past 3 months. It is a great way to assess your overall glucose control.
Fasting Plasma Glucose (FPG): FPG is used to assess glucose levels after a 12-hour fast, and is generally measured first thing in the morning. If your blood sugar levels are high after 12 hours of not eating, this is a sign that your body is not able to regulate blood sugar levels effectively.
Oral Glucose Tolerance Test (OGTT): OGTT is also performed after a 12-hour fast. Following the fast, you drink a high-glucose liquid. Your blood glucose levels are then measured at different intervals to assess how your body is processing glucose.
Triglycerides: A blood triglyceride test assesses the amount of fat in your bloodstream. High triglyceride levels are associated with insulin resistance and metabolic syndrome.
Cholesterol: An increased cholesterol, specifically high LDL is associated with metabolic dysfunction and insulin resistance.
What Are Natural Treatments for Insulin Resistance?
1. Get Adequate and High-Quality Sleep
Getting adequate high-quality sleep is important for a number of functions in the body, but recent research has shown it is especially important for healthy metabolic function. It is recommended to aim for 7-9 hours of high-quality sleep, and getting less than 5 hours of sleep per night has been shown to decrease insulin sensitivity, increase sugar cravings, and is considered a risk factor for developing insulin resistance.
Some tips to improve sleep quality and quantity include:
- Going to bed and waking up at the same time each day
- Avoiding screens and bright lights 1 hour before bed
- Avoid using the bed or bedroom during the day
- Creating a consistent evening routine
- Sleeping in a dark room
- Avoid napping during the day
- Limiting caffeine intake, especially later in the day
2. Engage in a Regular Exercise Routine
Exercise is one of the best ways to improve your insulin sensitivity. Exercise helps to move sugar into the muscles for storage, with benefits lasting 2-48 hours after exercise. Both cardiovascular and resistance training have been found to be beneficial, so the best kind of exercise is the type that you enjoy, and will participate in on a regular basis.

In addition, some weight loss can perpetuate even more weight loss, which can lower your risk of insulin resistance. Studies have also found that exercise has a positive impact on insulin sensitivity, independent of weight loss. It is generally recommended that adults engage in 150-300 minutes of low-intensity or 75-150 minutes of vigorous exercise per week.
3. Reduce Your Stress Levels
Research has demonstrated a link between chronic stress and insulin resistance and metabolic dysfunction. Many people have a number of stressors in their modern life, including relationships, finances, work, and family. It is important to identify chronic sources of stress and work on stress reduction and stress management techniques.

The link between stress and insulin resistance is due to the release of a number of stress hormones in stressful situations, leading to an increase in blood sugar. Historically, an increase in these stress hormones would mobilize fat and glycogen stores, increasing blood glucose, and allowing us to react to a physical threat, but because modern stressors rarely require a physical response, this increase in blood glucose is not used to energize our fight or flight response, meaning the glucose is not being used. Repeated stress can lead to a constant rise in blood sugar, leading to an increased risk of insulin resistance.
Some activities that have been shown to reduce stress levels include:
- Meditation
- Journaling
- Breathwork
- Yoga
- Exercise
4. Focus on a Healthy Diet
Nutrition is a key component of maintaining a healthy weight and preventing or reversing insulin resistance. A diet based on whole foods, including fruits, vegetables, nuts, seeds, and high-quality protein has been shown to be most beneficial for blood sugar regulation. Some foods to include daily are:
Fruits and vegetables: These are rich in vitamins, minerals, antioxidants, water and fibre. Vitamins and minerals are key for proper cellular and metabolic function, and water and fibre work together to slow digestion, blunt blood sugar spikes and increase satiety.
Soluble fibre: Soluble fibre is found in food such as beans, legumes, oatmeal, whole grains, sweet potatoes and Brussels sprouts. Soluble fibre is a type of carbohydrate that your body can not digest, instead it helps to bulk up stool and feed the bacteria in your gut.

Apple cider vinegar: Apple cider vinegar has increased in popularity over the past few years, mostly due to its ability to increase insulin sensitivity in those with insulin resistance and type 2 diabetes. A simple way to incorporate apple cider vinegar into your meals is to start meals with a small salad with a dressing of olive oil and apple cider vinegar.
Low glycemic carbohydrates: When choosing carbohydrates, it’s important to select carbohydrates with a low glycemic load. Some smart choices include green vegetables, non-starchy vegetables, sweet potatoes, berries, whole grains, and full-fat dairy. In addition, it’s important to limit high glycemic types of carbohydrates, including refined sugars, refined grains, processed foods, and sugary drinks.
When building a meal, it is important to build a balanced plate. A rule of thumb is to include a complex carbohydrate, a high-quality protein, a healthy fat, and a source of fibre in every meal. Eating all of these components together will help to slow the digestion of the meal, preventing a high blood sugar spike.
5. Maintain a Healthy Weight
Excessive weight, particularly in the belly area, has been associated with an increased risk of insulin resistance and increased risk of type 2 diabetes. A study by Johns Hopkins University found a weight loss of 5-7% correlated with a 54% decrease in the risk of developing type 2 diabetes. A combination of stress management, regular exercise and a healthy diet will help to aid in maintaining a healthy weight.
6. Herbs for Insulin resistance
A number of herbs have been shown to increase insulin sensitivity. They can be taken as teas, tinctures, or added to meals. Herbs that have been found to increase insulin sensitivity include:

Fenugreek seeds: These seeds are high in fibre, helping to slow digestion, and control blood sugar spikes. Many clinical trials have shown that fenugreek seeds have helped to decrease metabolic symptoms in individuals with both type 1 and type 2 diabetes.
Turmeric: Turmeric contains curcumin, a powerful antioxidant and anti-inflammatory. It has been shown to aid in insulin sensitivity by reducing sugar and free fatty acids in the blood.
Cinnamon: Cinnamon has been shown to help lower blood sugar levels and improve insulin sensitivity. It has also been shown to improve overall metabolic markers, including fasting glucose, cholesterol, triglycerides and liver enzymes.
Ginger: Ginger has been shown to increase insulin secretion, helping to lower blood sugar levels after a meal. It has also been shown to increase insulin sensitivity.
7. Nutraceuticals for Insulin Sensitivity
Chromium: Chromium is naturally present in many foods including meat, grains, fruits, vegetables, nuts and spices. However, in its concentrated form, it has been shown to improve insulin sensitivity and lower blood sugar levels.
Magnesium: Magnesium is used by the body’s insulin receptors, and a magnesium deficiency has been associated with insulin resistance. Taking magnesium supplements may help to improve insulin sensitivity in those with low magnesium levels.
Resveratrol: Resveratrol is naturally found in the skin of grapes and berries. In its concentrated form, it has been shown to improve insulin sensitivity.
Conclusion
In short, insulin resistance is a complex condition that can have profound effects on an individual’s health. However, there are many natural treatments to help manage and reverse inulin resistance. It is best to work with a healthcare provider to find out what treatments are best for you.
Source: Annex